Balancing magnesium (Mg) and vitamin D properly is essential for maintaining healthy organ functions. Vitamin D helps to regulate calcium and phosphate balance for healthy bones [2-7]. Skeletal muscles, heart, teeth, bones, and many other organs require magnesium to sustain their physiologic functions. This is where it gets tricky: magnesium is needed to activate vitamin D. Abnormal levels of either of these nutrients can lead to serious organ dysfunctions [8-13].
Magnesium activates more than 600 different enzymes, and influences calcium levels throughout the body [14]. It’s essential for stabilizing cell function, RNA and DNA synthesis, and cell repair, as well as maintaining cells’ antioxidant status. In addition to all of this, it’s an important cofactor for activating a wide range of transporters and enzymes [14,15 A].
Even when intracellular levels are low, the body will take magnesium from bone and tissues to keep the levels normal. And as this is a life-or-death situation, testing serum Mg is not an accurate method of determining the body’s need for this mineral.
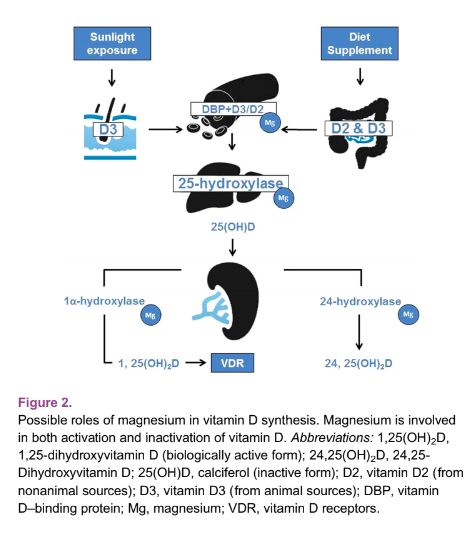
Vitamin D needs to be converted from its inactive form, 25-OH D, to active 1,25 OH D before it can act.The conversion is dependent on magnesium.
Magnesium, Vitamin D, and Their Symbiosis
People who are aiming to increase dietary magnesium can choose to eat morealmonds, beans, bananas,egg yolk, broccoli, tofu, brown rice, pumpkin seeds, soy beans, cashews, and oatmeal. It’s important to note, however, thatmagnesium content in food has declined from 25-80 percent compared to levels before 1950. This mineral is often lost from foods during processing, as well as from nutrient depletion in soil.
Vitamin D requires magnesium to convert it into its active form, and it’s also involved in D’s binding protein, as well as its inactivation.
Magnesium deficiency results in reduced levels of active vitamin D. Patients who are low in vitamin D and are supplementing should have their levels checked to ensure vitamin D is being utilized effectively.
Studies have found that women who consumed the highest amount of Mg possible (320 mg per day) achieved higher bone density and lowered their risk of osteoporosis. Biochemical features of reduced bone breakdown were seen in women who consumed magnesium citrate for only 30 days.
Related:Vitamin D Deficiency’s Role in PCOS and Hashimoto’s Thyroiditis
Minerals’ Roles in the Body
The two nutrients together also play a strong role in better health with metabolic disorders like insulin resistance and fat generated inflammation. In general, we perform both an RBC magnesium level and vitamin D level test in the clinic to ensure women are receiving the optimal amount of this crucial vitamin as per their needs.
High levels of 1, 25 vitamin D will substantially shorten the amount of time 25 OH vitamin D (stored vitamin D) stays in the body. Large variations in calcium intake can also produce variations in parathyroid hormones, which can cause 1, 25 OH vitamin D to vary as well.
When it comes to measurement, remember that calcitriol(1-25 OH Vitamin D)is a reactively produced hormone, and can be high when 25 OH vitamin D is low. Your body will raise calcitriol quickly if it sees the need to raise blood mineral levels (for example if dietary calcium is low). This hormone can be interesting to measure repeatedly over time, along with PTH, RBC Mg, serum zinc, copper, iron marker status, and 25 OH vitamin D however looking at this test alone will not provide an accurate view of nutrient status.
Article References:
- Anne Marie Uwitonze, BDT, MS; Mohammed S. Razzaque, MBBS, PhDRole of Magnesium in Vitamin D Activation and FunctionThe Journal of the American Osteopathic AssociationMarch 2018;Vol. 118:181-189.doi:10.7556/jaoa.2018.037
- Dusso ASUpdate on the biologic role of the vitamin D endocrine systemCurr Vasc Pharmacol2014;12(2):272-277.doi:10.2174/157016111131199900262
- Brown RB, Haq A, Stanford CF, Razzaque MSVitamin D, phosphate, and vasculotoxicityCan J Physiol Pharmacol2015;93(12):1077-1082.doi:10.1139/cjpp-2015-00833
- Razzaque MSBone-kidney axis in systemic phosphate turnoverArch Biochem Biophys2014;561:154-158.doi:10.1016/j.abb.2014.06.0314
- Razzaque MSPhosphate toxicity: new insights into an old problemClin Sci (Lond)2011;120(3):91-97.doi:10.1042/CS201003775
- Razzaque MSThe FGF23-Klotho axis: endocrine regulation of phosphate homeostasisNat Rev Endocrinol2009;5(11):611-619.doi:10.1038/nrendo.2009.1966
- Razzaque MSFGF23-mediated regulation of systemic phosphate homeostasis: is Klotho an essential player?Am J Physiol Renal Physiol2009;296(3):F470-476.doi:10.1152/ajprenal.90538.2008
- Jahnen-Dechent W, Ketteler MMagnesium basicsClin Kidney J2012;5(suppl 1):i3-i14.doi:10.1093/ndtplus/sfr1638
- Meintzer RB, Steenbock HVitamin D and magnesium absorptionJ Nutr1955;56(2):285-294.9
- Lynch HT, Lemon HM, Henn MJ, Ellingson RJ, Grissom RLVitamin D-intoxicated patient with hypoparathyroidism; hypercalcemia, acute cerebellar ataxia, and eeg changes: magnesium sulfate therapyArch Intern Med1964;114:375-380.doi:10.1001 /archinte.1964.0386009010901110
- Reddy P, Edwards LRMagnesium supplementation in vitamin D deficiencyAm J Ther2017;doi:10.1097/MJT.000000000000053811
- Nellis JC, Tufano RP, Gourin CGAssociation between magnesium disorders and hypocalcemia following thyroidectomyOtolaryngol Head Neck Surg2016;155(3):402-410.doi:10.1177/019459981664459412
- Haq A, Svobodova J, Imran S, Stanford C, Razzaque MSVitamin D deficiency: a single centre analysis of patients from 136 countriesJ Steroid Biochem Mol Biol2016;164:209-213.doi:10.1016/j.jsbmb.2016.02.007
- Swaminathan RMagnesium metabolism and its disordersClin Biochem Rev2003;24(2):47-66.15
- Noronha JL, Matuschak GMMagnesium in critical illness: metabolism, assessment, and treatmentIntensive Care Med2002;28(6):667-679.doi:10.1007/s00134-002-1281-y

