I gave this talk at the 2017 PCOS Challenge symposium, and am now delighted to be able to share it with all of you via YouTube!Learn why PCOS is a special condition requiring a medical approach that takes different systems, different times in life, and each woman’s unique needs into consideration.(For those of you who would prefer to read the transcript instead, just scroll down.)
Transcript:
Hi everyone, it’s great to be here today again.
I’m alwaysso impressed with everyone who comes to the symposium, and how dedicated everyone is to PCOS. This year we have some amazing things going on with the Congress, so I think our future is really bright. I want to talk today about the future of medicine for women with PCOS, because I think things are going to change quite a bit. I want you to think back, if this has happened to you, or I just want you to imagine that you’ve been having a lot of problems with your hormones, which I don’t think will be very hard for any of you to put yourself into that position.
You’ve been searching, and searching for answers as to why you have a irregular periods, why you have acne, or why you have hair growing on your face, and nobody’s really been able to give you an answer to that. You go to a doctor, a new doctor, and you get an ultrasound, and you get some blood work, and you get a call from your doctor, and he says, “Okay, I need you to come into the office.” You’re like, “Okay, I’m finally going to get some answers, I’m going to find out what’s wrong with me.”
You’re sitting there in the office, and you’re anticipating, “I hope it’s nothing serious, what’s the doctor going to say?” The doctor says, “You have PCOS,” so you’re like, “Okay, that’s good to know, at least I have a name for what’s wrong, and I’m going to do something about this,” right? You’re like, “Okay, great, so what do I do?” The doctor says, “Well, there is not a lot you can do for this, but here’s a pamphlet.” You’re like, “Okay, great,” so you take your pamphlet, you take it home.
You’re like, “Okay, that’s helpful,” and then you get a prescription for the birth control pill, or maybe Metformin. You’re like, “Okay, that’s good too, but what else can I do?” The doctor says to you, “Well, just lose weight.” You’re like, “Oh no,” and so basically, you go home, and your kind of feeling bummed, right? Has this happened to anyone? The day after I made this slide, someone posted on my Facebook, and this is exactly the day after I made this slide, she posted, “I got diagnosed with PCOS, I was given a pamphlet, and a prescription for the pill, and I went home, and I don’t know where the pamphlet is, and I never took the pill, and like what do I do?” Right?
Integrative Medicine
We’re left without anything to do to help ourselves.
We don’t even get any support, and I’ve been in this position myself, because I have PCOS, I went through years of having problems, and it’s just a condition which is underserved, there’s not enough help, and there’s not enough knowledge within the healthcare professions. I want to talk first about what is integrative medicine.I’m going to use Duke University’s definition of integrative medicine, because they have an amazing groundbreaking integrative medicine centre within their facility.
What they say is:
“Integrated medicine is an approach to care that puts the patient at the centre, and addresses the full range of physical, emotional, mental, social, spiritual, and environmental influences that affect a person’s health.” It puts the patient at the centre, so doesn’t that sound awesome, and then it goes on to say, “Employing a personalized strategy that considers the patient’s unique condition, needs, and circumstances. It uses the most appropriate interventions from an array of scientific disciplines to heal illness, and disease, and help people regain, and maintain optimum health.”
It’s using the most appropriate interventions from an array of different scientific disciplines.This is not “alternative” medicine, this is … We’re using what works at the right time from what we know in science.
Why is PCOS Particularly Suited for this kind of Medicine?
PCOS is a condition that’s a little bit different from other conditions, and for this reason, it’s particularly suited for integrative medicine. The first reason is that it’s a lifelong condition, so it never goes away. From the time that you’re a child, there are some signs of PCOS within your hormones, of the metabolic hormones we see in children.
Then adjustment of care is required at different stages of life, so it’s a condition that evolves, and changes actually quite profoundly throughout a woman’s life. The other thing is that it affects the entire body, so it doesn’t just affect our hormones. So many people think of it is an infertility condition, and it’s just not: it’s an endocrine condition. It affects the endocrine system, the mental emotional level, the reproductive system, the skin, the cardiovascular system, the metabolism, and the immune system.
It affects everything in our bodies, so we need everything to be considered. We can’t just focus on one thing, we have to look at women with PCOS as whole people, and look at their entire lives to really be able to help them. It’s also impacted by external factors, such as stress, environmental agents, nutrition, and diet, and exercise, and activity, so of many disorders, PCOS responds to diet quite profoundly, but it’s also impacted by environment. We see a lot of the endocrine disruptors, they can induce PCOS in animal studies, so there’s a lot of environmental impact, so that’s important for us.
What do we Know About the Root of PCOS?
Where does it come from? It’s definitely genetic, so who here has a family member with PCOS, or diabetes? Yeah, most of us do, and we know that it’s genetic, there have been many genes that have been isolated to PCOS. The next thing with it, is there’s insulin resistance, so there are definitely metabolic problems in PCOS: we see that even in lean women who have it. It’s more profound than in other women of the same body mass index, as there’s more insulin resistance.
The other part of it that’s at the root, is inflammation, so all women with PCOS have inflammation. I’m going to talk to you more about that, and inflammation is systemic, so it’s throughout our entire bodies, and it affects everything. Can anyone guess what this is? I’m a bit of a science nerd, my undergraduate was in cell and molecular biology, so I like looking at little things, and this is actually a picture of adipose tissue. It’s not the adipose issue of a Smurf: it’s actually not blue, our adipose tissue isn’t coloured. This is a scanning electron microscope image that’s coloured for emphasis.
We’ve always have thought of fat tissue as just being a storage, or storage tissue, where we just put fat in there, and it’s taken out whenever we need it, it’s just like an inert tissue. Well, that couldn’t actually be further from the truth. Here is our fat, and what we know now, is fat is an endocrine organ. It is functional, and in PCOS, there are a lot of problems with this endocrine organ.
Dysfunctional Fat Tissue
One of the things that fat does, is it regulates appetite, and energy balance through a hormone called leptin, and that goes up to our brain.It regulates our blood pressure, it regulates new blood vessel formation, it regulates insulin sensitivity, and blood sugar control, it regulates inflammation, and autoimmunity, metabolism of fat, insulin sensitivity, and nutrient transport, so as you can see here, fat is not just a storage tissue, it’s functional, and in PCOS, there’s a difference in the way our fat cells function, and they see this in children before they have any hormones from puberty that will show the signs of PCOS.
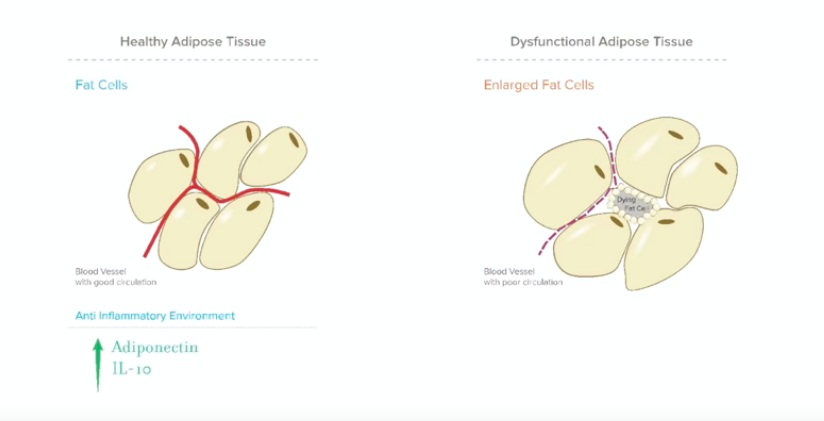
You’ll see this dysfunctional fat tissue, so here’s our healthy fat tissue, and as you can see, there are blood vessels going through it, so fat, compared to other tissues, and organs, it doesn’t have great circulation. It has some, but it’s not fantastic. So there are some blood vessels going through the fat tissue, and a healthy fat tissue actually produces anti-inflammatory hormones such as adiponectin, and they find that children who develop PCOS later, have lower levels of adiponectin.
It also secretes anti-inflammatory cytokines, which are signalling molecules, and these, this is IL-10, so healthy fat tissue has benefits for us. When we’re looking at dysfunctional adipose tissue, we see this in PCOS. This is one of the central things that you’re going to see. We’re good at storing energy, so one of the reasons that PCOS has survived throughout the ages, despite it causing infertility, is that it’s a very efficient condition. We’re good at storing fat, we’re good at storing energy, and we hold onto that, and we know how hard it is to lose weight.
Inflammation in Fat Tissues and How It Affects Us
Our fat cells become enlarged more easily, and store fat more easily. When the cells are enlarged, it blocks off the circulation, there’s just not as much good circulation, and the fat cells in the inner tissue actually can die. When that happens, what we start to see, is an inflammatory environment. The cells in the middle start to die, the immune system has to come in, and clean it up, and the fat cells also leak fatty acids. This causes inflammation, it causes the secretion of different kinds of inflammatory cytokines, and then we have low adiponectin, and this is a completely different environment.
All of this, your fat is throughout your body, it’s around your organs, it’s everywhere, so this inflammation, it’s everywhere in your body, and this is the chronic low-grade inflammation that we see in PCOS. I just want to show you again, geeking out on some electron microscope pictures here, and this is just one example of what inflammation can do in our body. This is our red blood cells, and that’s a platelet on the right, okay? This is a healthy person who doesn’t have any major inflammation in their body, so everything looks pretty calm, it looks nice.
Then we add IL-6, which is one of these inflammatory cytokines, and what you’ll see is look at all the platelets that came over there, right? They’re starting to form clots, this is just one thing that happens with inflammation, but it’s pretty profound, and then we’re seeing a close up here, so you can see the platelets start grabbing onto the red blood cells, and start causing clots. You’ll see even the surface of the red blood cells start to change when it’s exposed to inflammation.
Then here’s another cytokine, the IL-8, and look at the change there in the bloodstream. This is what chronic low-grade inflammation looks like in the blood, and this is there for years before anyone develops diabetes, this goes everywhere throughout our bodies. It affects every single thing in our body, as you can imagine, it’s a pretty profound problem. Does anyone think that you can help inflammation with food, or diet? Raise your hand if you do. Yeah, so you guys are right, you absolutely can.
How Food Affects Health
Food makes a big difference from a lot of different levels. Firstly, the amount, and the type of food, and the calorie density matters. Also, the quality of the food, and its inflammatory properties matter as well. Anything that adds more inflammation is going to make matters worse, obviously. We don’t want to add extra inflammation into what we already have. We’ve changed a lot in medicine, and since I’ve been in practice, there have been profound changes in the way that medicine is going with respect to diet and nutrition.
People used to think it didn’t make much of a difference, but now everyone is changing their mind on that.We’ll go back to 2013. ASRM, which is the biggest group of reproductive specialists in the US, they had a committee opinion titled, “Optimizing Natural Fertility.” It stated that there is little evidence that dietary variations, vitamin-enriched diets, antioxidants, or herbal medicines improve fertility. That was not very long ago; that was four years ago, so now they seem to have changed their mind quite a bit.
They say now, there are emerging epidemiologic data demonstrating that diet may influence reproductive health outcomes. Furthermore, translational work with human specimens and animal models lends biologic plausibility to the epidemiologic data, particularly in the context of female reproductive diseases associated with inflammation, including PCOS, and obesity. This is a very conservative group, and they now have changed their opinion, and believe that the anti-inflammatory diet is very important, and we see over, and over again, that it makes a big, big difference.
Does anyone want to guess what this is? Anyone? A sea anemone? It looks like a sea anemone, right? Again, it’s coloured to make it look more noticeable, and to show the difference between the parts.This is our small intestine. This is the brush border of the small intestine, so we can see here, these are what are called villi: the little blue brushes that are coming up, and that’s where we absorb our food. We absorb our nutrients through there, we absorb vitamins, and minerals, and as you can imagine, inside the small intestine, there’s lots of stuff going through there, right?
Intestines and the Immune System
There’s all kinds of food, there are some bacteria, the small intestine is one of our barriers to the outside world. It’s almost like the outside of the body, even though it’s inside. We have to be careful what we take up, we can’t take up everything, right? We can’t just absorb randomly everything that comes through there, we have to be picky about that, right? Does anyone know what these green things are? They’re called Payer’s Patches, so these are very large immune cell clumps, they’re large pieces of immune tissue.
A large proportion of our immune system is in our small intestines. It makes complete sense, because our immune system is our defender, we have to know what’s there, and we have to stop anything from coming in that shouldn’t be there. We also have to mount defenses against infections, and so our immune system is very vigilant right there in the small intestine. When you’re putting food in there, your immune system sees it, and it says, “Okay, what is that?” If it seems that it’s something that’s potentially harmful, it’s going to mount a response against that, that’s its job.
The amount of these Payer’s Patches, it’s quite large, it takes up a lot of surface area, so this is another reason that our food can influence our inflammation levels. Now that I’ve just given you a way to stand back, and look at how PCOS affects our body as a whole, how it’s really a systemic condition, and we have to address it through many, many different modalities for health. I just wanted to go through some of the common integrative modalities, because when we think of integrative medicine, we definitely include conventional medicine in there, and then we also add on other professions that can help.
Helpful Supplements
Some of the more common integrative approaches that we use are supplements. We have a lot of supplements that have really good evidence for them, including N-Acetyl-Cysteine, which is an antioxidant, that’s a precursor to glutathione. There’s a lot of studies for its benefits in PCOS.
Myo-Linositol, you’ve probably all heard of these. These are one of my favorites, they actually are similar to Metformin, they improve insulin sensitivity, and inside ourselves, Myo-Linositol is the main messenger for insulin.
Resveratrol, which is from grapes, is similar to the antioxidants in red wine. It’s also anti-inflammatory, so you’ll see a lot of them are anti-inflammatory that are beneficial.
Omega-3 fatty acids, again, these are beneficial for inflammation, consistently shown to reduce inflammation.
Then vitamin D. Vitamin D is a very, very important vitamin for the functioning of our immune system. It’s anti-inflammatory, and if you’re low in vitamin D, it promotes an inflammatory environment.
Exercise, and lifestyle are also very important, so psychology, counseling, acupuncture, electro acupuncture… there’s a researcher in Sweden who has devoted her entire life to studying this, Elizabet Stener-Victorin, on ovulation induction, and any kind of stress reduction is often helpful, and then nutrition, and diet, so foods that we’re eating. There are many different diets that can help with PCOS. There is no one correct diet. There are diets that work for different people with PCOS, and the ones that are studied commonly, include the ketogenic diet, the Mediterranean diet, the low glycemic index diet, or in our clinic, we use the food insulin demand diet, which is an evolution of the glycemic index, and then the low carbohydrate diet.
There are many options, and not everything will work for everyone. There’s no perfect diet, so I just wanted to show you how fast this is all moving, just so you can get an idea of it.
Recent Advances in PCOS
What I did, was I went to PubMed, which is where you search for clinical trials, and I searched for all of the new integrative interventions for polycystic ovary syndrome in the past year, and this is what we found. There are 106 new studies on PCOS, and nutrition, or diet. There are 91 new studies on PCOS, and complementary medicine. 88 new studies on dietary supplements. 33 new studies on PCOS, and exercise. 56 new studies on PCOS, and mood. 15 new studies on PCOS, and acupuncture.
This is for one year. There might be a little bit of overlap within some of these, but this is all for PCOS within one year, and this does not include any other research on PCOS. It does not include scientific research on the condition at all. This is just complementary approaches, 398 studies in the past year, and it doesn’t include research on insulin resistance for example, or hormones, or pituitary function, or thyroid, so all of the things that could impact PCOS.
This is a large body of evidence, and it’s growing rapidly, and don’t you want to be able to take advantage of all that? I know I do. I’m going to go through some of the studies that we’ve seen in the past year, these are just recent ones, there’s so many more, and I would never have time to go through all of it, it’s vast, and it’s important to be able to know how to read the studies, and to see if they’re actually legitimate, and well-designed. One of the studies that I thought was very interesting this year that came out, is about vitamin D and the dosing.
Vitamin D and Dosing
This is something I’ve seen in my practice as well. They compared two different doses of vitamin D. 60 participants, and this is in PCOS.They were in three groups, receiving either 4000, 1000, or placebo, and what they found, was that the 4000 dose improved the glucose metabolism, and lipid profiles more than the 1000 dose. The reason for this, is actually that there’s a very large range of vitamin D, so if you ever look at the levels, I know we use different units in Canada, but the range is extremely large, and just being at the bottom of the range often isn’t most optimal for most people.
People taking 4000 are more likely to get into the middle of the range, and then therefore to have more of an anti-inflammatory effect on them. There’s some other studies that have come in on vitamin D this year, so vitamin D and evening Primrose oil for PCOS. This is a randomized, double-blind placebo-controlled trial, 60 vitamin D deficient women with PCOS, and they found that compared to the placebo group, the women in the supplementation group had increases in vitamin D of course.
Plasma total glutathione, so glutathione is our antioxidant. Glutathione stops the damage of inflammation, so when inflammation is there, what’s the problem with it? It can damage our tissues, it can damage our cells, glutathione is our protector, it quenches oxidative stress from inflammation, and then there were significant decreases in triglycerides, VLDL, total high density lipoprotein cholesterol ratio, and Malondialdehyde. Malondialdehyde is a measure of oxidative stress. It’s not measured that often, there are some labs where you can get this done, but it’s an overall measure of oxidative stress, so the lower this is, the better.
Mineral Depletion Inflammation
Then we can look here at minerals, and what I find, is that there’s a lot of mineral deficiency in PCOS. The reason is that when there is insulin resistance, there’s an increased need for minerals. This a study on magnesium, zinc, calcium, and vitamin D. We have 60 women, they were randomized into two groups, and treated with 100 mg magnesium, 4 mg zinc, 400 calcium, 200 vitamin D, or placebo twice a day. What they found was after the 12 week intervention, compared with the placebo, the group on the minerals had reductions in hirsutism, HSCRP, which is an inflammation marker, and plasma Malondialdehyde.
Again, the oxidative stress is better, and a significant increase in plasma total antioxidant capacity. We’re seeing that minerals improve inflammation as well, and mitigate the damage that inflammation can cause. I’m going to do one here which was based out of Stanford University Clinical Research Center, again 2017, and this is on food. What they did was, they had two groups, and they replaced carbohydrates with fat, and they kept the calories the same. There are a lot of people who believe that it doesn’t really matter what you eat, right? It’s only the calories that really matter.
We’re sort of changing our minds on that: there are a lot of different things that go into what goes on with our metabolism. There were two groups of women who were given these diets, and they found one of them was 60 percent carbs, and 25 percent fat, and the other group was 40 percent carbs, and 45 percent fat, same calories every day. The glucose did not change. How many of you have been told that you don’t have diabetes, your glucose is normal, so nothing’s wrong with your metabolism?
Yeah, this is a big problem, because it’s not the same thing. Diabetes, and insulin resistance are related to each other, but diabetes is the end point: the insulin resistance goes on for a long time before you’ll develop any kind of diabetes, so their glucose did not change, however, the insulin concentrations were 30 percent lower on the lower-carb, high-fat diet. The reason for this is that fats don’t stimulate insulin release very much, and this is why many people find success with the low-carb, high-fat.
It’s not for everyone, but it definitely lowers insulin levels, and it promotes satiety. It’s always interesting to see the calories remain the same, and we’re still seeing that change in insulin. Obviously, any way that you can lower your insulin, you’re going to teach yourselves to be more sensitive. The lower the insulin, the more receptors your cells are going to have to put on the surface to get insulin to take the message from it. They also noted beneficial changes in lipid profile.
Insulin Resistance and Inflammation
With the lipids, triglycerides is the most important one to look at, but LDL, VLDL is also really important to look at as well. Let’s look at Omega-3 fatty acids. Omega-3 fatty acids I think are a staple when you have PCOS. They are very anti-inflammatory. It’s not the same as eating fish: they’re taken therapeutically in a clinical dose to reduce inflammation, and then this study is combining them with vitamin E. We had 68 women with PCOS, and they were given 1000 mg of omega-3 with 400 IU of vitamin E, or placebo for 12 weeks.
What they found, was there were improved indices of insulin resistance, total, and free testosterone, and this has been found in other studies as well, the same exact outcome. The reason again, is it’s anti-inflammatory, so when we’re looking at inflammation, we’re working on insulin resistance. The less inflammation, the better our cell membranes behave, and the more insulin sensitive we are.
I just wanted to go back to geeking out on microscope pictures with you, so this was actually fun to do all these microscope pictures, I just love it. Here’s our hair, right? This is an up close picture of hair, this is healthy hair, so who has experienced hair problems? I have, yeah, it’s common, right? We all experience hair problems, whether that be thinning, well not everyone, but a lot of us. Thinning hair, or maybe the hair is falling out rapidly, you’re getting thinning at the front, Androgenetic Alopecia, and this is really because of Androgen excess, but also inflammation affects our hair too.
Here we see someone with high cholesterol, and diabetes, this is not someone with Androgen excess, this is just to show you the metabolic effects on our hair. This is inflammation we’re looking, it’s severe of course, because they have high cholesterol, and diabetes, but that’s a big difference in the way the hair looks. Although part of our hair loss with PCOS is androgenetic, there is a big part of it that’s also metabolic, and inflammatory.
This next picture is with fish oil, and also diabetes, and high cholesterol.You can see some major improvements there, and what they found, is the fish oil group, they had a higher concentration of minerals in their hair, so the inflammation actually was impacting the entry of minerals into the hair, and as you can imagine, our other tissues are affected in a similar way. Then probiotics, so thinking back to the picture of the intestine, and then those Payer’s Patches, you can imagine that the bacteria that you put into your intestines make a difference too.
Supplementation
Your immune system’s really good at recognizing bacteria, as you can imagine: it’s made to do that. It’s made to look out for bacterial pathogens, and so it’s very reactive, and it can be reactive in a positive way as well when we’re looking at probiotics. We find that many probiotics can have systemic anti-inflammatory effects, specific strains especially. This is a study that just came out as well, in 2017, looking at probiotics, and the effects on weight loss, glycemia, and lipid profiles.
It’s a double-blind, randomized controlled trial. Supplementation for 12 weeks in 60 women, and favorable effects on weight loss, insulin resistance, triglycerides, and VLDL. Absolutely, your gut can impact inflammation. As you can see, it’s because of the effects on the immune system. Those bacteria promote beneficial changes in our immune system, and that trickles into our bloodstream. Then we can go to lifestyle, and herbal medicine, and this is another one just from this year.
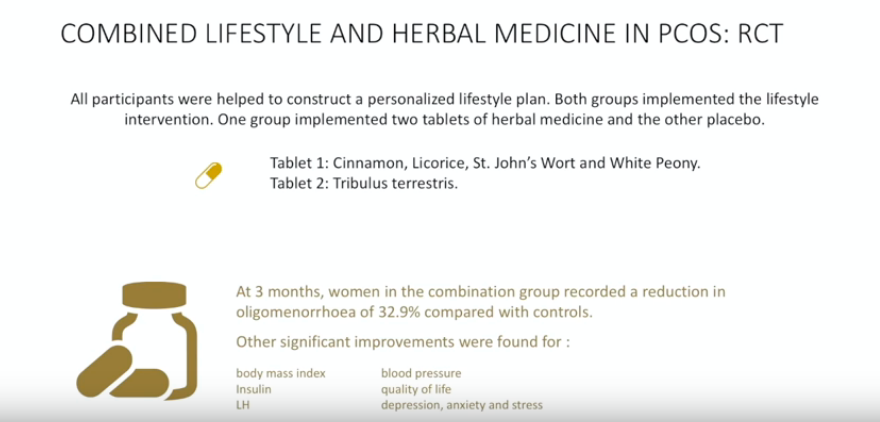
Herbal medicine is often very helpful for hormonal issues with PCOS, because many herbs actually have hormone-like actions. In this study, all of the participants did a lifestyle plan, so they were all doing lifestyle changes at the same time, both the placebo group, and the group on the herbal medicine. One group did the herbal medicine, and the other did a placebo. These were the herbs that they used, and these are commonly used actually in PCOS: tablet one is Cinnamon, Licorice, St. John’s Wort, and White Peony, and then tablet two was Tribulus.
Cinnamon, we know, helps with insulin sensitivity.
Licorice is anti-inflammatory, and does anyone know who should be careful when using licorice? High blood pressure, right. It can increase your blood pressure, so if anyone has hypertension, always beware and try not to use licorice.
St. John’s Wort, which actually helps primarily with mood, but also has anti-inflammatory effects, it also interacts with a lot of medications. Definitely not something to take without a healthcare practitioner monitoring that.
White Peony is one of the more researched herbs for PCOS that has anti-androgenic properties.
Tribulus Terristris is another herb that is used often for PCOS: it has hormone-regulating properties, and it’s also used an adaptogen, so it helps protect our body against stress. It reduces the perception of stress by the brain, so what happened was, the combination group, they recorded a reduction in oligomenorrhoea, meaning their periods came more regularly, by 32.9 percent, compared to the controls. They also had some improvements with body mass index, insulin, LH, blood pressure, quality of life, depression, and anxiety, and stress.
There are improvements for lifestyle medicine of course for both of these, but it seems that the herbal medicines offer additional improvements.
Then chromium, so chromium’s been used for many, many years for insulin sensitivity, and blood sugar regulation. It’s a really important mineral when we’re looking at metabolism. They did a systematic review this year, which means they take a whole bunch of studies, and look at them, and analyze them, and see if chromium is actually beneficial.
What they found was that the chromium picolinate does have beneficial effects on decreasing BMI, fasting insulin, and free testosterone. Then, so this is getting to be a lot of stuff, right? This is only a little bit of what happened in the past year, but I’m just showing you how vast it is. There’s a lot of things that could be benefited from, and if you have practitioners that understand this, and know how to read it, and can help you, and offer you support, and work together with everyone, you’re going to be able to benefit from a lot of different information we’re learning.
Green tea, green tea is a cool supplement, because it’s anti-inflammatory, so you can get those same benefits from drinking green tea. It also is an antioxidant, so it’s able to quench oxidative stress, and it’s also beneficial for our metabolism. Most likely, primarily, because of its benefits as an antioxidant. It also contains L-Theanine, which is good for stress, and it’s calming. Green tea, they took a double-blind randomized controlled trial of 60 women, and they took 500 mg capsules of green tea extract twice per day for 12 weeks, and what they found was that if the woman had a high body mass index, and PCOS, the green tea helped with weight loss, a decrease in fasting insulin, and a decrease in free testosterone, all of these things go together.
Now, these are not major changes, right? They’re things that can augment what you’re doing with your diet, and your lifestyle.
Then we have Vitex, which is probably one of the most well-known supplements for women’s hormones, and it’s one that there’s a lot of confusion as to how to use it, and who it’s beneficial for. Here we have a study on Vitex versus Metformin, which is interesting, because Vitex we often think of as more of a hormonal regulator, and Metformin is definitely for metabolic health and insulin sensitivity.
What they did, was they combined the two, but the thing with Vitex, is it has many, many more actions on the brain than it actually does on the ovary, so when you get into studying Vitex, you’ll see that it has really profound effects on dopamine in the brain, which is one of our neurotransmitters that helps us pay attention, but it also regulates a lot of other things in the body. Then it also has a lot of effects on the opiate receptors in the brain, and those have been found to be a problem in PCOS.
Here’s a double-blind randomized controlled trial of 60 women, and they did 3.2 to 4.8 mg of Chasteberry dry extract, depending on their weight, once per meal, for three months, versus 500 3, times a day, of Metformin. What they found, was that they had similar effects on menstrual cycle regulation, the length, and the number of pads used. More side effects were reported in the group using Metformin, which is we all know about that, it tends to cause side effects like within the gastrointestinal system.
Vitex does not really, so I guess what I’m trying to show you guys, is that there are a lot of different things that you can do to help your health, and we don’t want to be hammering a screw in when we can use something more suitable as a tool, and I think that we need to figure out what are the different areas that we want to improve with our health, and then to use the right tools at the right time, and work together, to really help us achieve our optimum health.
Final Thoughts
If you could go back now, and you’re in that office, and you’re sitting there waiting for your diagnosis. You’re like, “Ah, what’s wrong?” Your doctor says, “Okay, you have PCOS.” You’re like, “Okay, so what do I do?” Your doctor says, “Well, here are some medication options that you can try.” You’re like, “Okay, that’s good to know.” They’re like, “Here’s the testing that you need to do.” You’re like, “Great.”
Then your doctor says, “I also have other people here that I’m working with that are going to help you too. I have a psychologist, and a counsellor and we’re going to work together to take care of your mental, and emotional health, and stress, and I have a naturopath who is going to be able to help you with supplements, and functional testing, and functional hormone tests.I have an acupuncturist who can help you with stress, and ovulation, and I have a dietitian who can help you with meal planning, and adjusting your foods to suit you, and I have a personal trainer who’s going to help you work out, who’s going to show you what are the right exercises for you to do, and who’s going to teach you how to build muscle, and reduce your insulin resistance.Then I have a health coach, who’s going to encourage you when you’re feeling down, who’s going to educate you, and help you whenever you need it.”
Wouldn’t this be good if we got this when we were diagnosed?How much better would we all be if we had this?PCOS isn’t just our ovaries, and it’s not just our fertility: it affects our entire bodies, our minds, it affects our families, our social life. It’s a profound condition that requires intervention on various different levels, and a lot of different support.
I just want to say thank you, because you guys are the ones that can make these changes, only you guys can ask for these changes, and you are the ones who are here, who are dedicated to helping women with PCOS. When you guys ask for things, that’s where changes happen from, it’s from the patients, so thank you.