The pregnenolone steal has been taught in the world of functional and naturopathic medicine for many years. Although it seems to provide a nice explanation of how stress can impact hormones it is important to re-examine its validity in an era where we have rapidly increased our knowledge.
What is the Pregnenolone Steal?
The pregnenolone steal is based on what seems to be a logical idea: the way that hormones are synthesized though the steroid pathway.
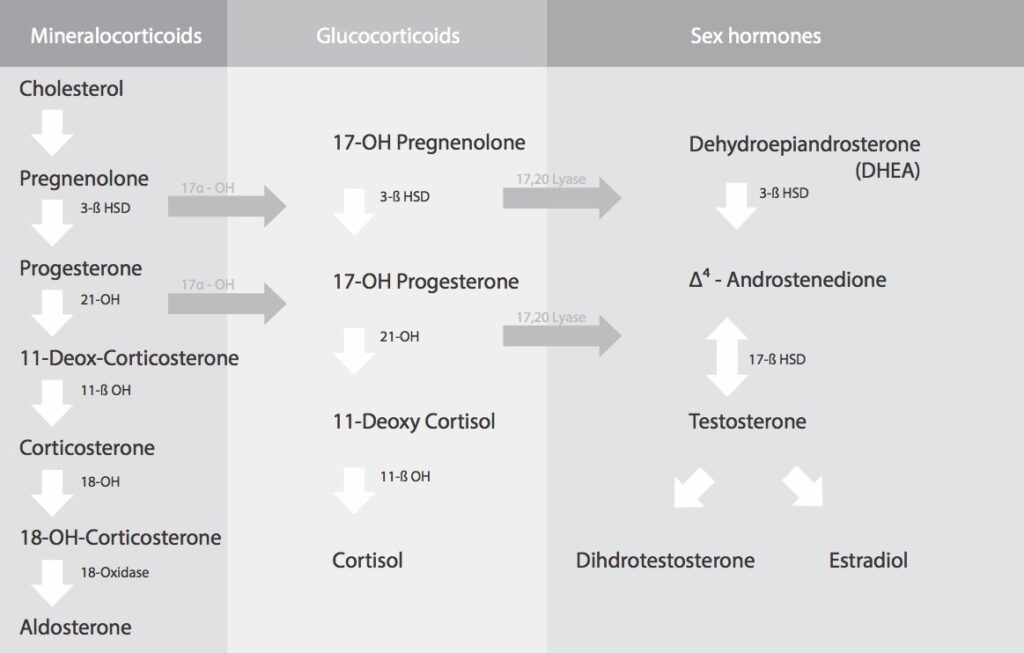
As you can see, pregnenolone is up at the top of the pathway, and all of the other hormones are synthesized from it.
According to this pathway, hormones like progesterone, testosterone, estradiol, and DHEA all come from a single pool of pregnenolone. Pregnenolone seems almost like a holding tank to make other hormones as needed.
The theory is that when cortisol is produced in excess (as in situations of stress), much of the available pregnenolone is used up to make cortisol, leaving less available for the formation of all of the other hormones.
Seems logical, right?
Let’s Look a Little Deeper
The steroid hormone pathway used to explain the pregnenolone steal looks quite complicated at first glance.
However, in reality, this pathway is an EXCEPTIONALLY oversimplified picture of hormonal regulation. It combines the production of hormones from completely different endocrine glands into one unit, for the purpose of simplicity.
It does not explain the complex regulatory mechanisms that govern the production of hormones. And ESPECIALLY not for ovarian hormones like estradiol and progesterone.
Different Compartments – Not a Gigantic Tank
Hormone production happens differently in different endocrine glands(and *inside* of different cells). I am going to use a few basic compartments (the adrenals and the ovary) to demonstrate this for you.
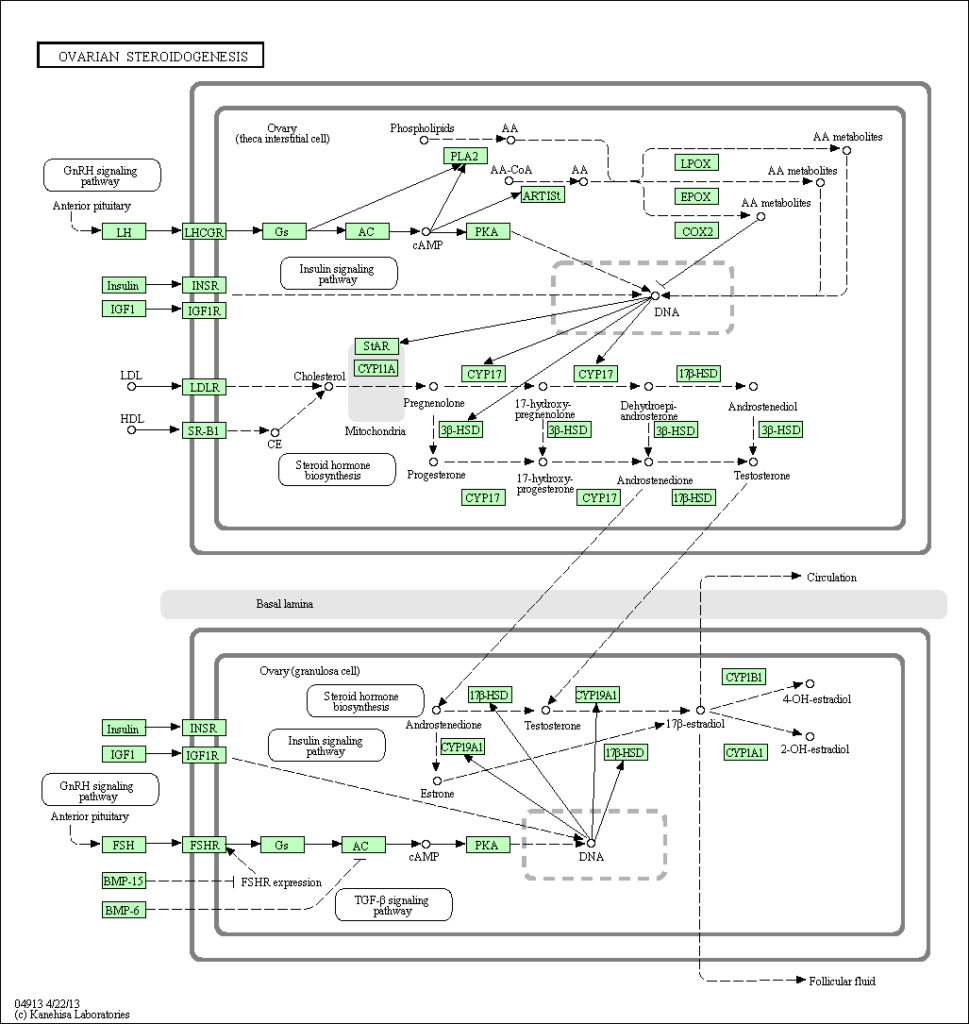
Let’s focus on the location of hormone production – the cell’s interior – in the mitochondria or endoplasmic reticulum. Each cell type (ie: adrenal zona reticularis, ovarian granulosa) has its own different pathway for the formation of steroid hormones which is triggered by a signal indicating a *need for that hormone*.
As aample, when cortisol is produced under stress or in the context of natural circadian rhythms, the pituitary gland releases ACTH and the adrenal zona faciculata cells take in cholesterol using special proteins and use it to make pregnenolone and convert it to cortisol. [1].
Unlike in the model of the pregnenolone steal, there is no one giant pool of pregnenolone that is drawn from at random. Although some pregnenolone leaks into the circulation, most of it is synthesized from cholesterol *inside* the cell. The conversion of pregnenolone into other hormones is determined by the type of endocrine gland itself, as well as enzymes, cellular signals, regulatory hormones and gene activity.
Hormonal Regulation in Women
When it comes to the ovaries, the pituitary hormone LH causes the uptake of cholesterol into and the production of pregnenolone within the ovarian theca cells that is then turned into testosterone. This testosterone is passed over to the granulosa cells. The influence of pituitary FSH on the granulosa cells causes testosterone to turn into estradiol.
The process of ovulation itself involves great change in the production of estradiol, testosterone and progesterone within the cells of the ovary in a cyclic pattern. This pattern is well-known to be regulated by the hypothalamus and the pulsatile release of GnRH from the brain. Progesterone is only produced by the theca cells after ovulation has occurred until the ovarian corpus luteum cells degenerate.
So Why Do Women’s levels of Estrogen and Progesterone Drop with Stress, Then?
There is a situation where stress will lower the production of estrogen and progesterone: Hypothalamic Amenorrhea. Again, however, this is not related to the stealing of pregnenolone precursor but is triggered by the brain’s perception of the environment in a larger sense.
If a high level of stress is perceived, the brain downregulates reproduction, by reducing production of FSH, and LH. Often this is accompanied by a drop in insulin and leptin (particularly if the type of stress is significant weight loss). Reproduction is a high-cost process for humans, not to be attempted when there is not enough food.
In these situations, the hypothalamus makes the “decision” to stop making ovarian hormones (meaning it decides not ovulate as reproduction would be risky). We can clearly see this mechanism though low pituitary LH and FSH levels. If the brain still wanted to ovulate – FSH and LH levels would rise to high levels.
There ather situations in which stress can reduce luteal phase progesterone, but again this appears to be caused by issues like endoplasmic reticulum stress in insulin resistance[3], and oxidative stress in inflammation[4].
So why do Hormones like DHEA-S go Down with Stress, Then?
It is often mentioned to clinicians that DHEA-S goes down with stress and illness because of increased cortisol synthesis (due to the pregnenolone steal).
However, it’s well known that DHEA-S levels naturally decrease markedly with age, and those who have lower levels of DHEA-S also have an increased risk of illness [5]. DHEA has been found to have a variety of benefits for many organs, including the function of brain [6].
It is thought that the decrease in adrenal androgens with age is caused by the glandular decline in the adrenal zona reticularis, known as “adrenopause”. However, the decrease in DHEA-S with aging happens independently from the adrenal’s ability to produce cortisol.
Also, iologic stress, from illness, inflammation, insulin resistance, or psychological stressors can affect DHEA-S levels[7][8][9] by altering adrenal androgen producing enzymes.
It has also been found that women’s DHEA-S levels temporarily increase during perimenopause/early menopause and then decline later, implying that the ovary affects adrenal hormone production as well. [10]
Dealing with Stress IS Important
As important as stress and cortisol dysregulation is to our overall health, the idea of the pregnenolone steal can be misleading if we are attempting to understand and treat the causes of hormonal issues.
That said, managing stress, sleep and circadian rhythm are truly foundational for our health and wellness, and they should always be emphasized if there is dysregulation of cortisol. In many endocrine cases, this may only take us to a certain point so it is important to understand the big picture.
To leave you with a super geeky idea of what happens in the hormone-producing theca and granulosa cells of the ovary, see the diagram below.
It’s pretty amazing, right?
Article References:
- Azziz, R., Nestler, J. E., Dewailly, D. (Eds.)Androgen Excess Disorders in WomenTotowa, NJ: Humana Press2007;https://doi.org/10.1007/978-1-59745-179-6
- Hu J, Zhang Z, Shen W-J, Azhar SCellular cholesterol delivery, intracellular processing and utilization for biosynthesis of steroid hormonesNutrition Metabolism2010;7:47.doi:10.1186/1743-7075-7-47
- Takahashi N, Harada M, Hirota Y, Zhao L, Azhary JM, Yoshino O, Izumi G, HirataT, Koga K, Wada-Hiraike O, Fujii T, Osuga YA Potential Role for Endoplasmic Reticulum Stress in Progesterone Deficiency in Obese WomenEndocrinology2017 Jan 1;158(1):84-97.
- Behera BK, Sharma CG, Singh SK, Kumar H, Chaudhari RK, Mahla AS, Das GK,Krishnaswamy NRelationship between endometritis and oxidative stress in the follicular fluid and luteal function in the buffaloReprod Domest Anim2016 Oct;51(5):844-7.
- Lois K, Kassi E, Prokopiou M, et alAdrenal Androgens and AgingEndotext2014 Jun 18;https://www.ncbi.nlm.nih.gov/pubmed/27510480
- Luque-Ramírez, M., Escobar-Morreale, H. F.Adrenal Hyperandrogenism and Polycystic Ovary SyndromeCurrent Pharmaceutical Designhttps://www.ncbi.nlm.nih.gov/pubmed/27510480
- Boudou P, Sobngwi E, Ibrahim F et alHyperglycaemia acutely decreases circulating dehydroepiandrosterone levels in healthy menClin Endocrinol (Oxf)2006 Jan;64(1):46-52.
- Woods AM, Judd AMInterleukin-4 increases cortisol release and decreases adrenal androgen release from bovine adrenal cellsDomest Anim Endocrinol2008 May;34(4):372-82.
- Crawford S, Santoro N, Laughlin GA, et alCirculating Dehydroepiandrosterone Sulfate Concentrations during the Menopausal TransitionJ Clin Endocrinol Metab2009;94:2945-2951.
- Woods AM, McIlmoil CJ, Rankin EN. Et alLeukemia inhibitory factor protein and receptors are expressed in the bovine adrenal cortex and increase cortisol and decrease adrenal androgen releaseDomest Anim Endocrinol2008 Aug;35(2):217-30.