Androgen excess is one of the most misunderstood, yet most central and powerful markers of PCOS. Many leading researchers now consider it an absolute requirement of the condition, and it is thought that even in women with PCOS who do not have apparent hyperandrogenemia, this is because levels are either undetectable by commonly used laboratory measures, or because clinical history has not been taken thoroughly.
As is the case with AMH (Anti-Müllerian hormone), androgen levels in women decline naturally and markedly with age.
Serum testosterone is commonly considered to be a biochemical marker for PCOS, but in women with clear signs of androgen excess, serum testosterone (T) is often normal. This is largely due to the low circulating concentrations of T in women, as well as the specificity and sensitivity of serum T assays, and the reduction of T with age.
More recently, T precursor androstenedione has been shown to be a more sensitive marker of PCOS-related androgen excess. Regardless of this, reference ranges still tend not to reflect the age-related decline in this androgen in women.
Adrenal androgens such as DHEA-S can be elevated in some women with PCOS, but this is clearly a specific subset: a woman’s age must also be taken into account for reference ranges.
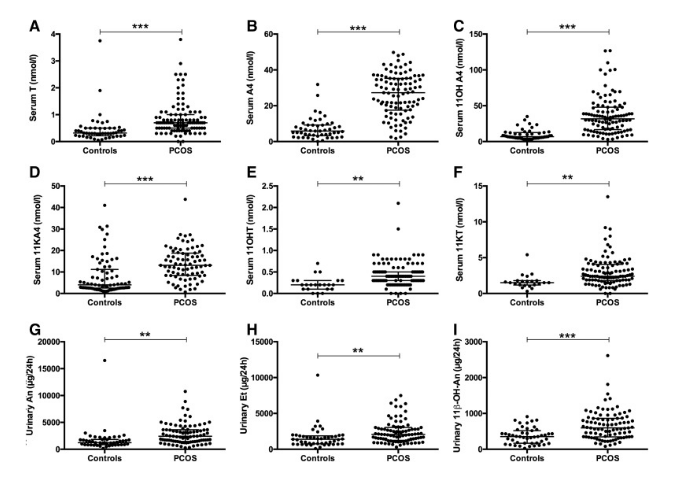
More recently, adrenal androgen metabolites have been investigated, and it has been demonstrated that 11OHA4—which isa major C19 steroid produced by the adrenal—is a major product of adrenal steroidogenesis(3). Although 11OHA4 has in the past been considered a dead-end product of adrenal steroidogenesis, it has been found that its downstream conversion through one of our steroid pathways generates 2 steroids: 11-ketotestosterone (11KT) and 11-keto-5α-dihydrotestosterone(4). These bind and activate the androgen receptor with affinities and potencies similar to that of testosterone and 5α-dihydrotestosterone, respectively (5).
Ref: J Clin Endocrinol Metab. 2017 Mar 1; 102(3): 840-848.
In fact, recent findings show that 11-oxygenated androgens make up the majority of circulating androgens in women with PCOS. These have a close correlation to markers of metabolic risk.
Due to this, androgen excess on the basis of normal serum testing in a woman who has either past or current clinical markers/dermatological signs of significant androgen excess.
Related Post: Treating Adrenal Androgen Excess
Clinical Notes:
This section is where clinical history becomes more important than biochemical assessment.A detailed history should be taken to confirm clinical signs of androgen excess, knowing that in PCOS, these often resolve with age.
Symptoms of Androgens in PCOS:
- Adult inflammatory acne persisting significantly past adolescence, particularly along the jawline.
- Hirsutism – (not including hair growth on the upper lip). Areas more commonly affected in PCOS-related androgen excess include the chin and chest. A woman’s chin (above and below) should be inspected to look for coarse hairs.
- Hair Loss: Androgenetic Alopecia. Androgenetic alopecia typically presents with the frontal hairline preserved and hair loss is located directly behind this area. At perimenopause, androgenetic alopecia may not relate to PCOS if no other patterns fit the condition due to loss of estradiol.
Lab Tests:
When serum or urinary androgens are being assessed, a woman’s age should always be considered.Reference ranges often include women throughout the entire reproductive lifespan and so are often inaccurate.Androgen levels in women decrease as women get older. In PCOS, levels may be at the “top of the range” in older women.
Serum:
- Total Testosterone
- Free Testosterone
- Androstenedione
- DHEA-S
- Dihydrotestosterone
- 17-OH Progesterone
Urinary metabolites (often provide a greater insight into androgen levels)
- Androsterone
- Etiocholanone
- Etiocholanone
- 5a-DHT
- 5a- Androstaneiol
- 5b-Androstanediol
- Epi Testosterone
- 11β-hydroxy-Androsterone
- 11β-hydroxy-Etiocholanolone (11βΟΗ−ΕΤ)