Certain foods in the standard American diet have been found to cause inflammation. Although some of these inflammatory food triggers are already known, it’salways interesting to learn new information about which nutrients may be causing the most problems. As more research is completed, we learn how we can improve the lives of women with PCOS through nutrition.
Many women with this condition have to contend with what is known as chronic, low-grade inflammation. This is associated with insulin resistance, weight gain, cardiovascular risk, and mood changes, as well as androgen hormoneexcesses (like testosterone).
What is Inflammation and Why Do We Have It?
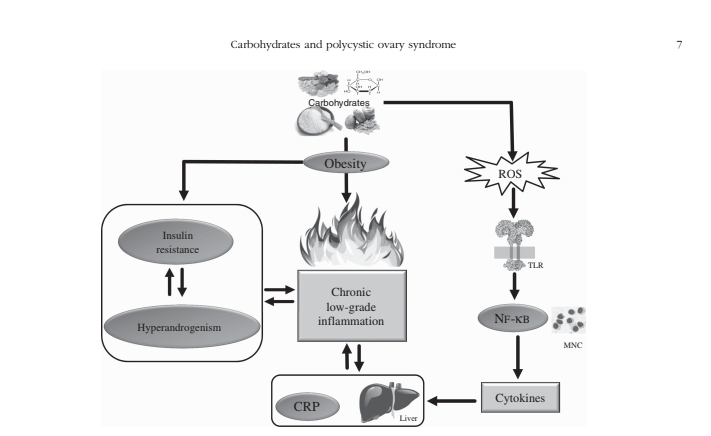
So, what is inflammation anyway? Our body’s innate immune system is our first line of defence against pathogens. This part of the immune system secretes chemical messengers—known as cytokines—as signals that trigger the inflammatory process whenever the body is threatened by bacteria or viruses. Inflammation is basically the immune system’s chemical messenger system that protects the body against invaders. It signals immune cells to sweep in and save the day.
It’s also known that in conditions like PCOS, this inflammation is present all of the time—not just when an invader is threatening the system. This constant inflammation, which is typically derived from insulin resistance and fat cell dysfunction, causes a constant stress to the body. It disrupts hormones, causing tissue damage and impacting every area of health, from mood to energy.
Inflammation After Eating
What most people don’t know is that inflammation tends to increase acutely right after eating a meal, and generally lasts for about 4-8 hours [2].
Unhealthy eating patterns as well as single food components have been shown to induce food-related inflammation.
We often think of “food allergies” or “intolerance” as being the source of this food-related inflammation. What most people are unaware of is that different macronutrients can have different effects on post-meal inflammation.
As dysfunctional fat cells accumulate in our “white” fat tissue—commonly seen in PCOS—these cells expand and leak inflammatory fatty acids. This causes cells to die and create debris in our bodies that needs to be cleaned up. Thankfully, our immune cells come to the rescue to clean this up, but unfortunately this leads to inflammatory cytokine release [3,4,5].
Related post:What Causes PCOS – Lipotoxicity and Inflammation
Carbohydrates and Inflammation
It’s well known that post-meal high blood sugar levels can induce oxidative stress and inflammation. But, do carbohydrates themselves cause inflammation?
Yes, and no.
When blood sugar levels rise, the immune system responds by producing an increased number of reactive oxygen species. These damaging chemicals are released as the cell’s internal powerhouses—the mitochondria—work to store and use the sugar through specific metabolic pathways.
The effect of eating carbohydrates—and how much inflammation is produced after a carbohydrate-heavy meal— really depends on two factors.
These are: how long blood sugar remains high after eating, and how high blood sugar levels get.
Additionally, anything that significantly increases insulin levels (especially if extremely elevated) will also contribute to further insulin resistance.
If a meal is lower in fibre, lower in healthy fats, high in refined carbohydrates, and has a high insulin index (or glycemic index) it will cause a relatively large spike in blood sugar after eating. The body then falls into a pro-inflammatory state as the mitochondria struggle to manage this excessive carbohydrate-derived energy.
Carbohydrates and PCOS
It is also important to remember that fructose—which has a low glycemic index—generates 100 times more reactive oxygen species than glucose, through completely different mechanisms in the liver. So, eating lots of fruit or sweetened foods are just as problematic for inflammation.
It is clear now that this pro-inflammatory state has emerged as a key contributor to the health issues found in women with PCOS [6]. PCOS-associated metabolic and ovarian dysfunction is made much worse by diet-induced oxidative stress and inflammation [7]. Studies too numerous to count show us that nutrition is one of the most powerful ways to reverse PCOS symptoms, and prevent chronic disease.
Inflammation and Testosterone in PCOS
Directly exposing PCOS ovaries to inflammatory cytokines also increases testosterone production. As a result, oxidative stress and inflammatory markers are highly correlated with circulating androgens in women with PCOS. [8]
How To Address Carbohydrate-Driven Inflammation in PCOS
Overall, chronic inflammation is a huge issue for PCOS. The good news is that different dietary approaches focused on healthy fats, lean proteins, non-starchy vegetables, and carefully selected carbohydrates can create significant improvement for women suffering from the many elements of this condition.
This is whythe nutrition program I’ve developed works so well for PCOS. It is not a standard “low carb diet”, but rather, it contains quality carbohydrates that are strategically included in carefully designed meals. These are always combined with optimal healthy fat levels, protein, and carbohydrates to stabilize and manage blood sugar, reduce diet-triggered inflammation and keep insulin levels under control.
Keeping PCOS-related metabolic issues at bay are all about what, how much, and when we eat.
This type of approach can successfully put a stop to the abnormally high blood sugar and insulin spikes that we often see in PCOS. As a result, we keep inflammation in check.
This type of nutritional approach not only makes fat loss easier (since abnormally high levels of insulin block the burning of fat), but also lowers the inflammation that triggers many of the common hormonal disruptions found in PCOS, like irregular cycles, hirsutism, acne, and hair loss.
Article References:
- Minihane AM, Vinoy S, Russell WR, et al.Low-grade inflammation, diet composition and health: current research evidence and its translationBr J Nutr2015;114:999-1012.
- Calder PC, Ahluwalia N, Brouns F, et al.Dietary factors and low-grade inflammation in relation to overweight and obesityBr J Nutr2011;106(Suppl. 3):S5-S78.
- Neale EP, Batterham MJ Tapsell LCConsumption of a healthy dietary pattern results in significant reductions in C-reactive protein levels in adults: a meta-analysisNutr Res2016;36:391-401.
- Galland LDiet and inflammationNutr Clin Pract2010;25:634-640.
- Escobar-Morreale HF, Luque-Ramírez M González FCirculating inflammatory markers in polycystic ovary syndrome: a systematic review and meta-analysisFertil Steril2011;95:1048-1058.
- Paniagua JANutrition, insulin resistance and dysfunctional adipose tissue determine the different components of metabolic syndromeWorld J Diabetes2016;7:483-514.
- González FNutrient-induced inflammation in polycystic ovary syndrome: role in the development of metabolic aberration and ovarian dysfunctionSemin Reprod Med2015;33:276-286.
- González FInflammation in polycystic ovary syndrome: underpinning of insulin resistance and ovarian dysfunctionSteroids2012;77:300-305.
- Luigi Barrea, Paolo Marzullo, Giovanna Muscogiuri, Carolina Di Somma, Massimo Scacchi, Francesco Orio, Gianluca Aimaretti, Annamaria Cola, and Silvia SavastanoSource and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndromeNutrition Research Reviews2018;